One day, Verna Earl Hamilton Grice discovered she could not walk up the driveway.
That was the first sign.
Later, she felt tremors on one side of her body.
Ten years ago, she was diagnosed with Parkinson’s disease.
That’s when she stopped painting.
“I got tired,” Verna, 88, says. “I didn’t do it for 10 years. It’s labor intensive. Susan kept on.”
That would be her daughter Susan Grice, 63, who shares Verna’s zeal for making art.
“She focused instead on trying to figure out the illness,” Susan says of her mother. “She went to support groups such as Power for Parkinson’s. They promote exercise.”
Verna: “I was just hanging on.”
Verna, a native of Lake Charles, La., nevertheless made significant progress. A return to painting has helped.
Susan: “Her doctor says she is in the top 1 percent of his patients.”
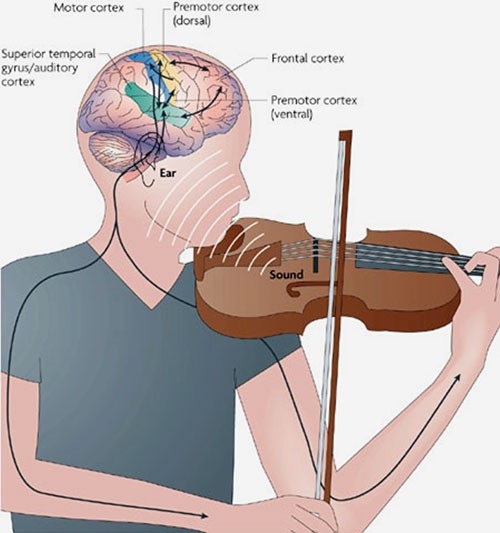
“I walk really well,” Verna says with a laugh. “If you walk well, they think you are OK. I have my ups and downs. My ups are longer than they were, because I am so busy painting these days. Just looking at the paint seems to help.”
In their airy home studio, Verna and Susan paint together on wood. They seal the paintings so they can be hung outdoors. Their subjects include images inspired by Old Masters, original ideas, nature and abstract arrangements.
As in the past, the mother-and-daughter team enjoys a steady demand for their output, which could be called garden art. They recently staged an exhibition that attracted more than 60 guests to their house and garden in Westover Hills.
“It makes me feel better, I noticed,” Verna says. “How did I start again? My dentist was going out of his way to be sweet to me — I hate going to the dentist — so I brought him one of my pictures. He loved the picture. He had to have two more. They hang in the dentist’s office for others to enjoy.”
“She came home and said, ‘Oh no. I’ve got to get painting. We’re back in business,’” Susan says. “Since then, we couldn’t stop.”
The Grice method
Susan and Verna make 24-by-24-inch paintings on 3/4-inch exterior plywood.
“It’s done directly on the wood,” Verna says. “We prime it and then seal it several times after painting.”
“It’s like making signs,” Susan says. “They last for years and years. We don’t tell the exact formula. It’s a secret. A carpenter friend makes the frames of cedar.”
Mother and daughter come to the project with similar artistic sensibilities.
Susan, former director of psychiatric nursing at Seton Shoal Creek, studied at the Glassell School of Art, the teaching institute of Houston’s Museum of Fine Arts.
As for Verna, she was artistic as a child in Louisiana. She painted a bit in high school. She followed that inclination to Mexico City, where she studied Spanish and art in 1948 and ’49.
“Diego Rivera and Frida Kahlo were very much around,” Verna says. “I remember seeing Diego’s mural at a hotel there.”
A child of the Depression, Verna did not expect much more from life than hard work.
Her father, Vernon Earl Hamilton, took whatever jobs he could land.
“I never knew what to say when they asked, ‘What does your Daddy do?’” Verna recalls. “There were so many things, since it was the Depression. I know he owned slot machines on the side. He put them in little bars around Lake Charles. He sold one to let me go to Mexico.”
Her mother, Ruth McLaughlin Grice, worked as a bookkeeper for an ice company.
“She went to work to get me braces,” Verna says. “Guess what? She was working till she retired. I never got my braces.”
Verna has one sister, Helen Ruth Garman, who at age 84 is a Ride Austin contract driver.
Even Verna’s Mexican adventure came with a practical work goal.
“I was hoping to get a job using my Spanish,” she says, “but couldn’t find one. So I worked for a construction company for a while, then went to Houston. That’s where I met my husband, a young lawyer named Harrison Marion Grice.”
The newlyweds settled down in southeastern Houston and raised three children: Susan, 63, Charles, 61, and Laurel, 54.
Verna did not stop working.
“I sold real estate for a while,” she says. “I was a bilingual secretary in Spain after my husband died and also a legal secretary. I worked for the National Treasury Employees Union and lived in Washington for eight years. I was marching with the union when the older President Bush tried to freeze employees’ salaries to pay down the national debt. I was arrested and handcuffed, stuffed into a paddy wagon and taken to jail. The one thing I remember is that the toilet in the jail is right out in the middle of the room. That’s punishment enough.”
The family moved to Austin’s Northwest Hills in Austin in 1975. She retired in 1996 as the assistant to her union’s president and purchased the Westover Hills home in 2001.
Why paint?
“I just got in the mood,” Verna says of her first adult painting 15 years ago. “I got bored with looking out at those bare fences around the patio. They needed some color. That’s when we started making groups of paintings.”
Susan started painting and selling art right after Verna started in 2004. They’ve sold more than 100 paintings, many of them at places that also sell architectural pieces or items for the garden.
Verna finds that Parkinson’s is only a partial barrier.
“With just about any disability, you can still paint,” Verna says. “If you find someone to help on some things, you can still enjoy the magic of painting.”
“You let me draw straight lines for you sometimes,” Susan interjects. “With her permission and very specific instructions, she will direct me to draw a line. It allows her to still paint, which is fantastic.”
Both Grices promote Power for Parkinson’s, the nonprofit support group that offers free exercise, dance and singing classes at locations in Austin, Round Rock, West Lake Hills and Lakeway.
“I started going when there were just a few things we could do there, and now there are hundreds of activities,” Verna says. “I swim laps. I play bocce ball. I boxed. I decided my body is not made for boxing. Age 88 is too old to dive into the mat.”
Verna does not paint to inspire others, but she’s gratified it might do so.
“I just want people to know that, at 88, you can still have some fun and enjoy life,” Verna says. “A lot of people with Parkinson’s think that this is the end. But you can slow it down. You realize how important your brain is. Don’t get me wrong. It’s a bear of a disease. But it is not hopeless. There are lots of things you can do. Do it, try it — and get creative with it.”
Click HERE to view the artwork. Article from Austin360.com.





Recent Comments