Symptoms of cabin fever go far beyond feeling bored or “stuck” at home. They’re rooted in an intense feeling of isolation and may include:
- restlessness
- decreased motivation
- irritability
- hopelessness
- difficulty concentrating
- irregular sleep patterns, including sleepiness or sleeplessness
- difficulty waking up
- lethargy
- distrust of people around you
- lack of patience
- persistent sadness or depression
Your personality and natural temperament will go a long way toward determining how cabin fever affects you.
Some people can weather the feelings more easily; they may take on projects or dive into creative outlets to pass the time and ward off the symptoms.
But others may face great difficulty with managing day-to-day life until these feelings pass.
What can help you cope with cabin fever?
Because cabin fever isn’t a recognized psychological condition, there’s no standard “treatment.” However, mental health professionals do recognize that the symptoms are very real.
The coping mechanism that works best for you will have a lot to do with your personal situation and the reason you’re secluded in the first place.
Finding meaningful ways to engage your brain and occupy your time can help alleviate the distress and irritability that cabin fever brings.
The following ideas are a good place to start.
Spend time outdoors
Research shows that time spent in nature is time well spent for mental health.
Not only does spending time outdoors boost your cognitive function, it may also help:
Depending on your reason for isolating, be sure to check all local regulations and avoid any spaces that are closed for safety or health reasons.
If getting outdoors isn’t an option, you could try:
- opening up your windows to let the outdoor breeze in
- adding a bird feeder outside your window to bring birds closer to your living space
- ordering or buying fragrant, fresh-cut flowers and placing them where you can see and smell them throughout the day
- growing herbs or small plants on a windowsill, patio, or balcony
Give yourself a routine
You may not have a 9-to-5 job to report to while you’re isolated, but a lack of routine can cause disruptions in eating, sleeping, and activity.
To keep a sense of structure, try to create a daily routine that consists of work or house projects, mealtimes, workout time, and even downtime.
Having an outline for your day helps you keep track of the trajectory of your hours and gives you mini “goals” to hit throughout the day.
Maintain a social life
So you can’t go to the movies or meet your friends for dinner. But you can still “meet up” with them — just in a different way.
Use real-time video streaming services, like FaceTime, Zoom, or Skype, to chat with your friends, colleagues, and loved ones. Face-to-face chat time can keep you in contact with the “outside world” and make even your small home feel a whole lot bigger.
Connecting with others who are in a similar situation can also help you feel that you’re not alone. Sharing your thoughts, emotions, and challenges with others can help you realize that what you’re feeling is normal.
Connecting with others may even help you find creative solutions to an issue you’re grappling with.
Express your creative side
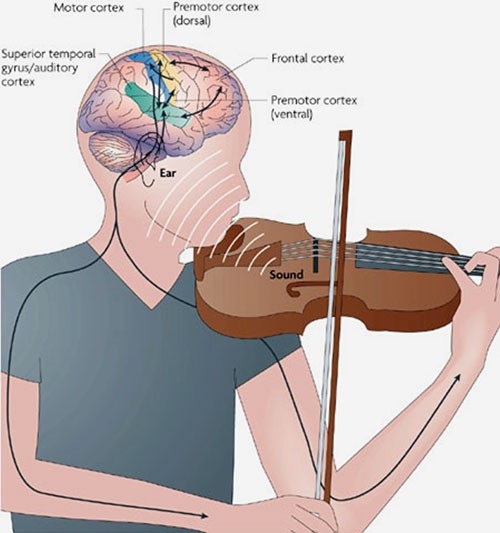
Did you play a band instrument in high school? Were you once interested in painting? Do you have stacks of vacation photos you once promised yourself you’d put in a scrapbook? Is there a recipe you’ve always wanted to try but never had the time?
Use your time in isolation to reconnect with creative activities that you’ve had to put on hold because life got too busy. Spending time on creative activities keeps your brain busy.
Keeping your mind occupied and engaged may help ward off feelings of boredom or restlessness and make the time pass more quickly.
Carve out some ‘me time’
If you live with others, feelings of cabin fever may be intensified by the nearness of other individuals.
Parents have responsibilities to children; partners have responsibilities to one another. But that doesn’t mean you shouldn’t have any time on your own.
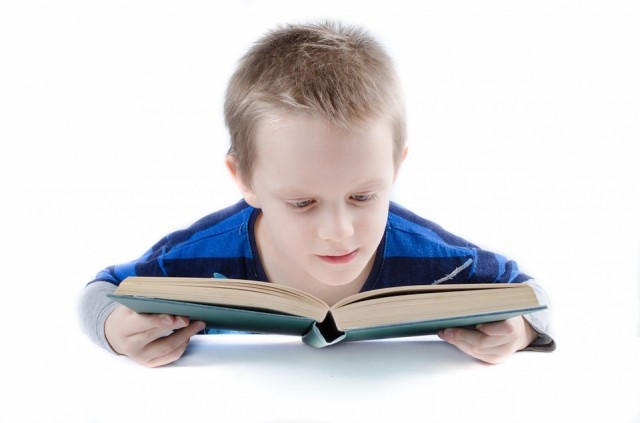
Give yourself time “away” from others to relax. Find a quiet place to read a book, meditate, or pop in some earbuds for an engaging podcast.
If you’re feeling stressed, you may even want to tune in to a podcast on mental health or anxiety.
Break a sweat
Research has shown that people who exercise regularly are less prone to anxiety than people who don’t exercise. That’s because physical activity lowers your body’s stress hormones, such as cortisol.
At the same time, exercise causes your brain to release endorphins. These neurochemicals can boost your mood and overall feeling of well-being.
If you can’t get outside, you can do a strength training workout at home using just your body weight or simple equipment, like dumbbells or resistance bands.
Or you can put together your own routine by focusing on a few basic but effective exercises, such as:
- pushups
- squats
- burpees
- lunges
- planks
If you need a more structured program, there are plenty of online exercise options on YouTube and through various exercise apps.
Chill out
Not every minute of every day you spend at home has to be planned. Give yourself some time to rest. Look for constructive ways to relax.
Mindfulness, deep breathing, and relaxation exercises may help you maintain your emotional health and balance feelings of isolation or frustration.
When to Get Help
Cabin fever is often a fleeting feeling. You may feel irritable or frustrated for a few hours, but having a virtual chat with a friend or finding a task to distract your mind may help erase the frustrations you felt earlier.
Sometimes, however, the feelings may grow stronger, and no coping mechanisms may be able to successfully help you eliminate your feelings of isolation, sadness, or depression.
What’s more, if your time indoors is prolonged by outside forces, like weather or extended shelter-in-place orders from your local government, feelings of anxiety and fear are valid.
In fact, anxiety may be at the root of some cabin fever symptoms. This may make symptoms worse.
If you feel that your symptoms are getting worse, consider reaching out to a mental health professional who can help you understand what you’re experiencing. Together, you can identify ways to overcome the feelings and anxiety.
Of course, if you’re in isolation or practicing social distancing, you’ll need to look for alternative means for seeing a mental health expert.
Telehealth options may be available to connect you with your therapist if you already have one. If you don’t, reach out to your doctor for recommendations about mental health specialists who can connect with you online.
If you don’t want to talk to a therapist, smartphone apps for depression may provide a complementary option for addressing your cabin fever symptoms.
The Bottom Line
Isolation isn’t a natural state for many people. We are, for the most part, social animals. We enjoy each other’s company. That’s what can make staying at home for extended periods of time difficult.
However, whether you’re sheltering at home to avoid dangerous weather conditions or heeding the guidelines to help minimize the spread of a disease, staying at home is often an important thing we must do for ourselves and our communities.
If and when it’s necessary, finding ways to engage your brain and occupy your time may help bat back cabin fever and the feelings of isolation and restlessness that often accompany it.
Article from Healthline.com






Recent Comments