This article from LA Times focuses on Linda Ronstadt, who was diagnosed with supranuclear palsy, a variant of Parkinson disease, in 2013.
Parkinson’s differences in women and men
There is growing evidence that Parkinson’s disease (PD) affects women and men differently. In this insightful review, published in the Journal of Parkinson’s Disease, scientists present the most recent knowledge about these sex-related differences and highlight the significance of estrogens, which play an important role in the sex differences in PD.
PD is a slowly progressive disorder that affects movement, muscle control, and balance. It is the second most common age-related, neurodegenerative disorder, affecting about 3% of the population by the age of 65 and up to 5% of individuals over 85 years of age. The risk of developing PD is twice as high in men than women, but women experience a more rapid disease progression and a lower survival rate.
“It is becoming increasingly evident that PD differs in women and men,” explained lead author Fabio Blandini, MD, Scientific Director of the IRCCS Mondino Foundation, National Institute of Neurology, Pavia, Italy. “Recent research findings suggest that biological sex also impacts on disease risk factors and, potentially, on molecular mechanisms involved in the pathogenesis of PD.”
This review meticulously examines the most recent knowledge concerning differences between women and men with PD including:
- Motor and non-motor symptoms
- Quality of life
- Genetic and environmental risk factors
- Pharmacological therapy of motor and non-motor symptoms
- Surgical procedures
- PD and steroids
- Impact of biological sex on pathophysiology
Recent research has shown that women and men have distinctive motor and non-motor symptoms as their PD progresses. Motor symptoms emerge later in women: tremor is a common first presenting symptom associated with recurrent falls and more severe pain syndromes with specific characteristics such as reduced rigidity, a higher propensity to develop postural instability, and elevated risk for levodopa-related motor complications. Conversely, male PD patients show more serious postural problems and have worse general cognitive abilities: freezing of gait—the most disabling motor complication of PD—develops later in men; however, men have a higher risk of developing camptocormia (abnormal severe forward flexion of the trunk when standing or walking). An ongoing clinical trial is evaluating the prevalence in PD and the biological sex impact on other postural abnormalities, such as Pisa syndrome (a reversible lateral bending of the trunk with a tendency to lean to one side), antecollis (dystonia of the neck resulting in excessive forward flexion), scoliosis (a sideways curvature of the spine), and deformities related to hands and/or toes.
Non-motor symptoms have been the subject of a study of over 950 PD patients, which concluded that symptoms such as fatigue, depression, restless legs, constipation, pain, loss of taste or smell, weight change and excessive sweating are more common and severe in women. Other studies have demonstrated that male PD patients have worse general cognitive abilities and male sex is the primary predictive factor for mild cognitive impairment and its more rapid progression in the severe stage of the disease. A diagnosis of PD with dementia has a greater impact on life expectancy of women than men; in addition, women show distinctive symptoms as well as differences in the response to pharmacological therapies and deep brain stimulation, and in their personal evaluation of the quality of life compared to men.
The authors note that the distinctive clinical features as well as the contribution of different risk factors support the idea that PD development might involve distinct pathogenetic mechanisms (or the same mechanism but in a different way) in women and men. They highlight the significance of estrogens, which play an important role in the sex differences in PD, providing disease protection as demonstrated by the similar incidence of the disease in men and post-menopausal women.
“Sex hormones act throughout the entire brain of both males and females and sex differences are now highlighted in brain regions and functions not previously considered as subjected to such differences, opening the way to a better understanding of sex-related behavior and functions,” added Silvia Cerri, Ph.D., head of the Laboratory of Cellular and Molecular Neurobiology of the IRCCS Mondino Foundation and first author of the article. She commented: “Neuroinflammation is an important piece of the pathogenic puzzle of PD. Current evidence suggests that the physiological role exerted by microglial and astrocytic cells could become compromised during aging, thus contributing to PD onset and progression. Since estrogens have anti-inflammatory properties, their actions throughout the lifespan could partially account for sex-related risk and manifestation of PD.”
By drawing attention to sex-related differences and disparities in PD, Dr. Blandini and colleagues hope this will further encourage the scientific community and policy makers to foster the development of tailored interventions and the design of innovative programs—for example in care practices—that meet the distinct requirements of women and men with PD. “Women diagnosed with PD are a sizable portion of the PD population, but their specific needs are still partially overlooked. The differences between women and men strongly suggest the need for a personalized (sex-related) therapy in PD,” concluded Dr. Blandini and Dr. Cerri.
Parkinson’s and depression: it’s not all in your mind
Depression is a very real and debilitating condition that many Parkinson’s disease sufferers experience. ParkinsonsLife guest writer Dr Nicola Davies explores the causes of and treatments for depression and Parkinson’s.
It’s well-documented that people who have been diagnosed with a chronic illness such as Parkinson’s are at higher risk of developing depression as well. Indeed, it’s estimated that 50% of people diagnosed with Parkinson’s will experience depression.
As Suma Surendranath, professional engagement and education manager at Parkinson’s UK, says: “Parkinson’s is a long-term progressive condition for which there is currently no cure, therefore a diagnosis can be a psychological blow for a person and those around them as they may well be concerned about what the future might hold.”
The following scenario is a common experience among many newly diagnosed Parkinson’s sufferers. First there is confusion: ‘What does this mean?’, ‘What can I do?’, ‘How will this impact me?’ Then the shock comes as the reality of the disease sets in and the impact that it will have on the rest of your life is realised. The shock gives way to grief and depression. The feeling that your life has ended and your hopes and aspirations have been shattered is less time than it takes to make a cup of tea. As one person with Parkinson’s told us, “When I was diagnosed, I came home and cried. I thought it was the end of my life.”
“There is evidence that suggests depression is an early symptom of Parkinson’s”
However, receiving a diagnosis for Parkinson’s isn’t the only factor that can cause depression in people with this condition – the very course of the disease changes the brain chemistry that usually keeps depression at bay.
Surendranath says: “Depression may occur amongst people with Parkinson’s as a result of the condition as dopamine, the neurotransmitter that becomes depleted with Parkinson’s, is [also] involved in motivation and a sense of reward.”
Experiencing depression after receiving a diagnosis of Parkinson’s isn’t a sign of emotional weakness or a flaw in character. Depression is caused by an imbalance of chemicals in the brain, which is what Parkinson’s is all about: low levels of chemicals in the brain.
There is evidence that suggests depression is an early symptom of Parkinson’s. Despite this, people with Parkinson’s aren’t routinely tested for depression and therefore might not receive treatment for the condition.
It remains unclear whether the medications prescribed to reduce the physical symptoms of Parkinson’s contribute or worsen symptoms of depression. It is also unclear how Parkinson’s affects pre-existing depression or how medication prescribed for Parkinson’s impacts pre-existing depression.
Surendranath says: “While medication, in the form of anti-depressants, can be beneficial to people with Parkinson’s it is still important to ensure that there are no adverse effects from medications interacting with each other.”
Words of hope
Depression is treatable even if it co-exists with other conditions. Depression is also limited in duration. Often, finding the right mixture and combination of drug therapy can improve both the physical symptoms of Parkinson’s and the symptoms of depression. However, it is important to know that the treatment of Parkinson’s must be comprehensive and include both the physical as well as the emotional symptoms.
Reaching out can also ease the depressive symptoms associated with Parkinson’s. As one patient told us, “I started meeting other people with Parkinson’s and it helped all of us to talk to someone who had the same condition.” There are many physical and online communities where other people with Parkinson’s can meet up virtually, or in person, and share their experiences with others who are feeling the same and suffering from similar symptoms.
Most importantly, you have to set a goal in for your life. Unless you have something to aim for, or something that drives you to get up every morning and face the day fighting, you will find yourself drifting through life. It is best to accept that you have Parkinson’s and move on.
Dr Nicola Davies holds a Master’s and a PhD in Health Psychology. She is a member of the British Psychological Society and the Division of Health Psychology. Article from ParkinsonsLife.
Nutrition-packed summer recipe for people with Parkinson’s
Jane McClenaghan, a nutritional therapist and author based in Belfast, Northern Ireland, runs cookery classes and diet clinics which help people living with Parkinson’s.
This two-course meal, from her book ‘The Vital Nutrution Cookbook’, is packed full of anti-inflammatory ingredients like cinnamon and ginger, a helping of fish for omega-3 and baked nectarines to offer an easy-to-swallow treat for dessert.
First course – Thai fishcakes with zingy salsa

Thai fishcakes with zingy salsa made by nutritional therapist Jane McClenaghan
Ingredients
5-7oz. white fish
4 scallions, chopped
1 inch fresh ginger, grated
1 tsp Thai green curry paste
1 egg, beaten
2 tbsp chopped cilantro
1 tbsp flour
Juice and zest of a lime
Black pepper
1 tsp coconut oil
Method
- Finely chop the fish and place in a large bowl with the spring onions, ginger, curry paste, fish sauce, egg and cilantro.
- Mix well and then stir in the flour, lime juice and zest and season with black pepper. The mixture may be a bit wet at this stage. You can add a bit more flour if you like.
- Divide into four generous portions. Put a little flour on your hands and form each portion into a ball. Flatten slightly and fry in the coconut oil for five to eight minutes until golden brown and cooked through.
- Serve with a green salad or my zingy salsa (below).
For the salsa
½ cucumber, finely chopped
½ red onion, finely chopped
2 medium tomatoes, chopped
1 red pepper, finely chopped
½ fresh chilli, finely chopped
2 tbsp fresh cilantro, chopped
1 tbsp chives, chopped
Juice of 1 lime
1 tbsp olive oil
Freshly ground black pepper
Method
- For the salsa, place all the ingredients in a bowl and mix well together. Season to taste.
- To serve, pile the salsa high on your plates alongside the fishcakes.
Dessert – Cinnamon nectarines with vanilla scented yogurt


Cinnamon nectarines with vanilla scented yoghurt by Jane McClenaghan
Ingredients (serves 2)
1-2 tsp agave syrup
2 nectarines, halved with stone removed
½-1 tsp ground cinnamon
½ vanilla bean
2 tbsp Greek yogurt
Method
- Preheat your oven to 350F.
- Drizzle a little agave syrup over each nectarine half and sprinkle with cinnamon. Cover with tinfoil and bake for 15-20 minutes until soft.
- Slice the vanilla bead lengthways and, with the tip of a sharp knife, scrape out the seeds and stir into the Greek yogurt.
- Serve the nectarines hot or cold with a drizzle of agave syrup and a dollop of the vanilla scented Greek yogurt.
Recipes are taken from Jane McClenaghan’s book, ‘The Vital Nutrition Cookbook’.
Article from Parkinson’s Life.
Do You Know How Lucky You Are?
While my grandkids were here last week, we read books every night before bed. And, of course, each night at least one book had to be by Dr. Seuss. The night before they left, we read “Did I Ever Tell You How Lucky You Are?“
It starts out by offering some rather sound advice:
“When you think things are bad,
when you feel sour and blue,
when you start to get mad …
you should do what I do!
Just tell yourself, Duckie,
you’re really quite lucky!
Some people are much more …
oh ever so much more …
oh, muchly much-much more
unlucky than you!”
Of course, Dr. Seuss then spends the rest of the book expounding on all the different ways the reader is lucky as a ducky.
Most people would agree that having been handed a diagnosis of Parkinson’s disease is anything but lucky. In fact, it can be downright scary. Even so, there are things to be thankful for. Things that cause you to pause and say, “I am so lucky” or “I am so blessed.” Things that take your mind off the unknown. Things that give you hope.
Today, I fell
I was puttering in my yard, trying to eradicate the wounded and the dead and replace them with the new. I stepped down on the shovel to finish digging the hole for a salvia plant, and I lost my balance.
It seemed as if I was falling in slow motion.
On the way down, all I could think of was hitting my head on one of the rocks that line the pathway. Some of them are sharp. I fell hard on my arm and then, with a rocking motion, came to a halt, my head never touching the ground. I waited a minute to assess the damage before trying to get up. No pain. No scratches. I was lucky. I was blessed. Given what could have been a terrible accident (considering the DBS wires tucked in my brain), I was indeed blessed.
Life is so beautiful
I went over to my grandson’s house yesterday to help him and his mom weed their backyard. When we had finished, he began yelling for his mom and me to “Come here. Quick! Come here!” He was jumping up and down (literally) with such joy on his face that I was certain he’d found a bug he’d never seen before. (Or perhaps George, “his” praying mantis, had shown up again.)
I approached where he stood, next to a small, bushy plant. He looked at the plant — a weed, by most standards — and with great excitement exclaimed, “It’s so beautiful!”
It was a smallish plant with little yellow flowers scattered here and there. To him, it was so beautiful.
Oh, how lucky I’d be if I could see the world through the eyes of a child. But wait! I did!
Oh, how lucky I am!
“Thank goodness for all of the things you are not!
Thank goodness you are not something someone forgot,
and left all alone in some punkerish place
like a rusty tin coat hanger hanging in space.” —Dr. Seuss
Caregivers: 8 Things Caregivers Need
It’s not uncommon for spouses to decide to leave when the other gets sick. I think it could be a matter of “having had it up to here” and then finding out the one you’ve “put up with” for so long now has a condition that will most likely make your life — and theirs — a lot more difficult. Parkinson’s may change the relationship between a married couple. Bonds between a father and son. Between a mother and daughter. Friends. It comes in and subtlety takes away the ties that once bound these relationships together.
The PD patient changes. They are physically familiar, but mentally and emotionally, they’re not the same. And the caregiver is left struggling with how to deal with this new role in life: taking care of someone else while taking care of themselves.
If you are a caregiver to anyone, first of all, thank you for your commitment and sacrifice. You might get hit, have to change yet another big girl or big boy diaper, clean up another spill, or wash another naked body, but we (your charges) appreciate you more than we might be able to say or show.
Following are eight little things you can do as a caregiver that will hopefully, make your role easier:
- Breathe deeply and when you get one free minute, do one thing that puts a smile on your face. Go out to the garden and breathe in the fragrance of a rose. Put on encouraging music. Read a short devotional. Fix a cup of tea. Scream. Screaming is highly underrated.
- Don’t focus on the what-ifs. They’ll defeat you most every time. Do focus on “now.” It may seem like a tremendous struggle at the moment, but things could be worse. Today may be one of the harder days, but when the clock strikes 12, it’s a new day. Something wonderful could be ahead, waiting to happen. Your patient may turn into a pumpkin! Don’t lose hope.
- If you don’t have one already, get a sense of humor. Without one, you’ll often despair. Find something funny in every day. You need to laugh.
- Get yourself into a support group locally or online. You may not think you need it, but you do. Especially as the road becomes bumpier. And it will get bumpier. Get some support in place now, as it will make things easier to deal with later.
- You need your friends. Don’t alienate them by thinking you can do this by yourself. Accept their invitations to help. Accept an hour off, washing the dishes, picking up some groceries, dropping the kids off at practice, or cooking your family a meal. Give yourself some slack and let your friends feel needed, because if they are offering to help before you have even asked, they may see your need better than you can.
- Try to think ahead. Your loved one’s mental faculties may not be so great anymore. A daily schedule may be useful, with a reminder for doctor’s appointments, visitors, special occasions, etc.
- Don’t beat yourself up. There will be good days and bad days. You may have more bad days now due to your new, unwanted role. And because this admittedly is an unwanted role, you feel like your life has been swallowed up along with the one you’re caring for.
You have thoughts of packing it in. Giving up. Throwing in the towel. Walking away and leaving the patient to fend for himself or herself. You’re tired, weary, spent, worn out. You want it to end and you feel guilty for thinking and feeling the way you do. And it’s OK. It’s normal. You’re caring for the one you’re grieving, while at the same time grieving what you’ve both lost already and what you could very well lose still. It’s OK to be frustrated, to go outside for a reprieve and scream. It’s OK to let the tears flow. Just remember: The one you love is in this fight with you, not against you. They just aren’t able to fight as they once did. Try to remember them as they were 10, 15, or 20 years ago when you laughed together and lived life together.
Also try to remember that if your husband could get out and mow the lawn again, he’d do it in a heartbeat. If the wife you care for could brush her own teeth and tie her own shoes, you’d both be ecstatic. Whatever you’re losing, they are losing as well. They’ve been dreading the days to come with a vengeance.
If they could, the one you are caring for would take this bitter cup from you. However, that cup may one day soon be empty, so enjoy it now while there is still some liquid left, even if sour at times.
The Story Changes, While the Message Endures
Parkinson disease was in the national spotlight recently with the passing of auto industry icon Lee Iacocca, as well as ESPN founder Bill Rasmussen’s recent announcement that he has been living with the disease.
Learn more about these two very different stories, and how Parkinson’s affected each of them.
Heel, Toe: Walking with Mindfulness
“Mindfulness isn’t difficult, we just need to remember to do it.” — Sharon Salzberg
The ability to walk is something many of us, myself included, have always taken for granted. Now that I have Parkinson’s disease (PD), something that used to come as a matter of course to me is starting to deteriorate. PD has adversely affected my left side more than my right side. I find myself tripping more, since I tend to drag my left foot.
Walking now requires my conscious thought
Going for a walk is now more of a mindful task than an exercise for me. I find it much more therapeutic to focus on how I walk and be in the present moment than to think about the future and how my PD may progress. With each step I take, I concentrate on repeating to myself, “Heel, toe.”
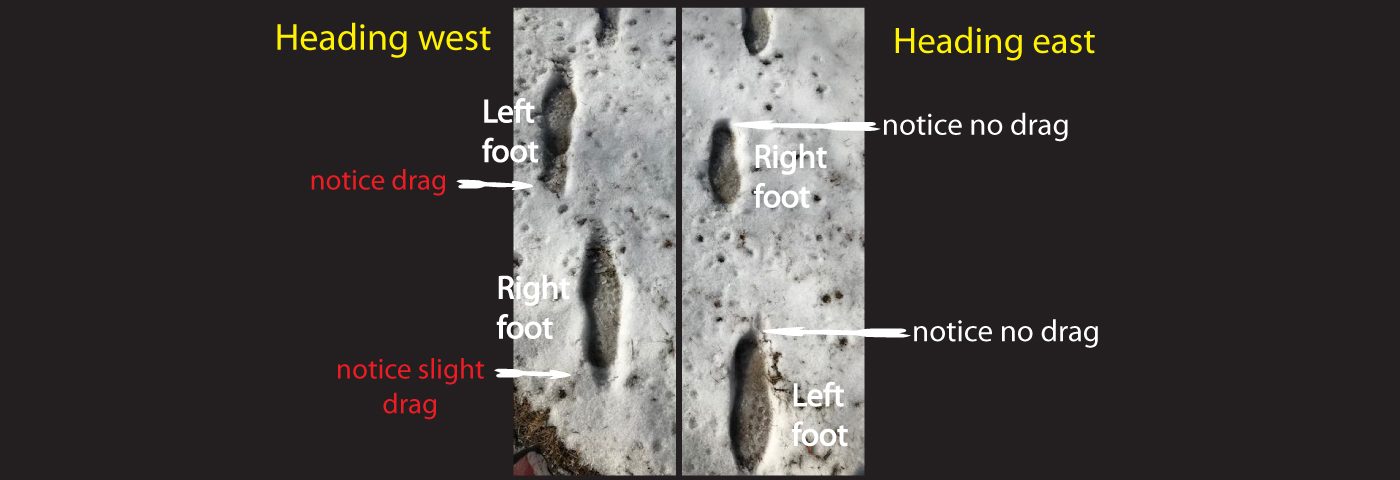
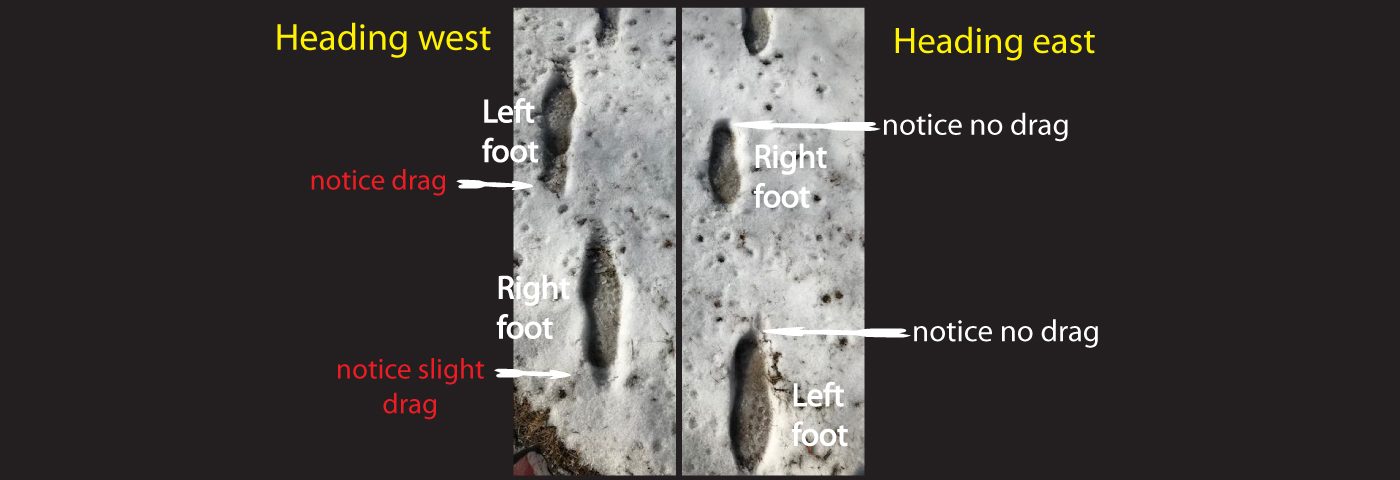
When there was snow on the ground, I decided to compare my walking steps when I did not focus on saying “heel, toe” with those from when I did. My footprints in the snow were very telling, so I took a photograph. On the left side of the photo are my steps when I was not thinking about my stepping patterns. You might notice that both feet show a bit of a drag in the snow. On the right side of the photo, as I moved forward, I really focused on flexing both of my feet and having my heel strike first. There are no signs of drag on either foot.
Am I putting too much thought into this?
Years of training to improve as a dancer and a cyclist have made analysis of my body movements come quite naturally to me. Whether it was improving my pedal stroke for more cycling power or perfecting my balance to do pirouette turns, I learned to be mindful and to be in touch with how my body was performing. Now I must use that skill to help myself be more attentive when I walk.
My neurologist says I tend to overthink things. I believe our greatest strengths can also be our greatest weaknesses. Sometimes, I do overthink, to the point of getting paralysis by analysis. However, I believe that mindful analysis of my PD symptoms (including my walking technique) is critical in helping me to create different ways of doing things that at one time (before PD) used to come as second nature to me.
IBM unveils fingernail sensor that can monitor PD
Recently IBM unveiled its latest innovation that could change the way how we monitor health. It’s prototype AI-powered fingernail sensor will let its users place the sensor over their fingernail to detect symptoms and track disease progression.
According to IBM, the innovation can help track cognitive functions in schizophrenics, check the effectiveness of medication in a person with Parkinson’s disease and even individuals’ cardiovascular health.
Although there are skin sensors that can monitor body activities, it is hard to place them on people with Parkinson’s disease as a majority of them are older patients with brittle skin and might lead to infection.
But by shifting the sensors to the nail, not only did they avoid the problem of skin rash that could arise from skin sensors, they were able to track the activities of hand for throughout the day which is a key factor in diagnosing degenerative neurological diseases such as in the case of Parkinson’s disease.
“Our fingernails deform — bend and move — in stereotypic ways when we use them for gripping, grasping, and even flexing and extending our fingers. This deformation is usually on the order of single digit microns and not visible to the naked eye,” said Katsuyuki Sakuma, from IBM’s Thomas J. Watson Research Center in New York.
The system consists of strain gauges attached to the fingernail and a small computer that collects data and communicates with a smart watch, which is equipped with machine learning models to rate bradykinesia, tremor, and dyskinesia which are all symptoms of Parkinson’s disease.
The AI-powered sensor monitors the bending and movement of a patient’s nail to calculate their grip strength. It then transmits the information which includes matters like nail wrap, motions, gestures, finger-writing, grip strength, and activation time from the wearable sensors to an off-finger device for interpretation and draws meaningful insight.
With this invention, IBM says that it is one step closer to materialising their longtime challenge of using AI to help clinicians monitor individuals in their natural environments. “By pushing computation to the end of our fingers, we’ve found a new use for our nails by detecting and characterising their subtle movements,” Sakuma said in closing.
Free and inexpensive resources to help on your Parkinson’s journey
We asked, and you answered! Here are a few of your favorite FREE or INEXPENSIVE resources and tips that you have found helpful in dealing with your Parkinson’s.
Barb in Davenport: I use the CALM app on my phone. It’s not free but it is so worth it. Check it out for high quality meditations, sleep stories, daily inspiration, etc.
Nancy in Mount Pleasant: Subscribe to “Brain & Life” magazine. It’s helpful and free!
Bruce in Kaukana: I have Parkinson’s and we use a free app called Life360. It allows you to add family members and you can see/follow them as they are driving or riding in a vehicle. It gives some piece of mind knowing you can see where a person is while driving. You can add your aging parents, young drivers, drivers with or without a disability.
Anna in Milwaukee: The “Every Victory Counts” manual from Davis Phinney Foundation. The digital version is free, or the print version is $5.50. The Parkinson’s Foundation offers their free Aware in Care kit as well.
Joel in Fond du Lac: The Parkinson’s Playbook by Robert W. Smith. It’s available on Amazon for $14 and includes some tips on lifestyle improvements and healing techniques.
Jason in Whitewater: WPA’s program last week in Janesville was great, and connected me to a local gym.
Susan in South Beloit: I used a music stand to put my heavier books on when I’m reading. Also, I go to the YMCA several times a week to take water exercise class. It’s refreshing, easy on my joints and a great way to make new friends.
Have more ideas to share? Email [email protected] and watch for a future article!
Recent Comments